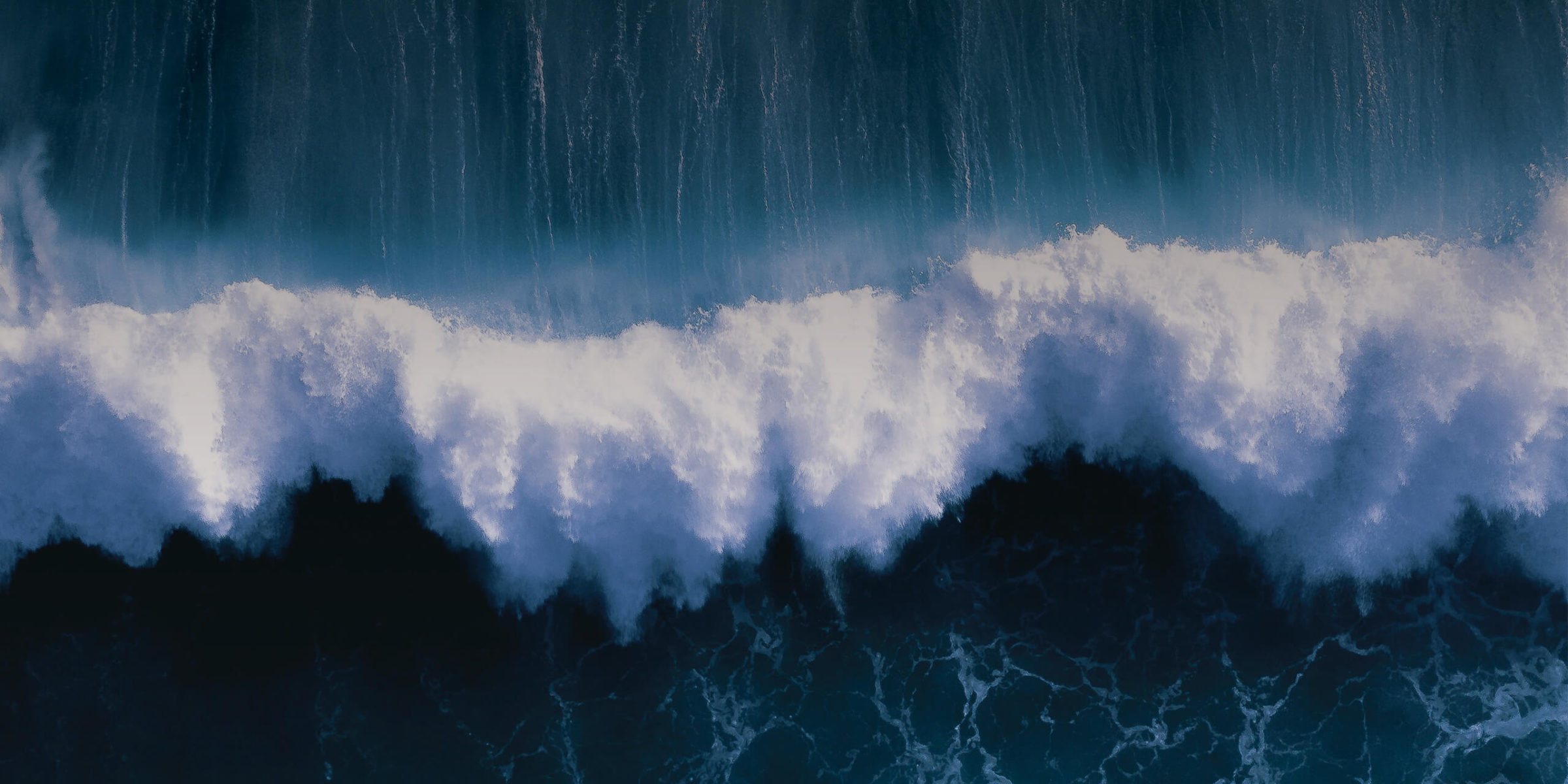
The Ripples and the Tsunami

Covid-19 has undoubtedly transformed our lives over the past 12-18 months. We have, of course, been focused on the short-term impact on individuals, the NHS and the economy, but what of the long term?
There are, of course, the ongoing implications of high numbers of cases in other countries and worries about emerging variants, but that’s not something we can control. From a healthcare perspective the ripples of Covid-19 will be felt for years, perhaps even decades.
NHS waiting lists are reported to have hit 4.7 million people, a 14-year high. The last time they were that long the new Wembley Stadium had just been completed, Apple had just released the very first iPhone, the Bank of England was bailing out Northern Rock and the final Harry Potter book was being released. Put like that, it’s a pretty significant backward step. When will the backlog be cleared? Even a betting man wouldn’t bet on it being anytime soon!
The impact of COVID-19 on primary care has been substantial. Cancer Research UK estimates that around 350,000 fewer people than normal were sent for an urgent suspected cancer referral during April-August 2020. There were around 60% fewer referrals in April 2020 compared with April 2019 and this had yet to recover in August 2020, with referrals still slightly lower than before the first lockdown.2 We all know that behind these data are patients who will be diagnosed later, with more advanced disease, poorer outcomes and ultimately excess mortality. Those are the hard facts.
There was much talk early on in the pandemic about increased suicide rates. Thankfully that doesn’t seem to have materialised, with a recent article in the BMJ confirming that suicide rates have not risen. That doesn’t mean though that there has been no impact on mental health. Suicide is, after all, an end-of-the-line sign of mental health. How many newly emergent mental health crises have there been that we are yet to fully measure?
Emptiness and stagnation
A recent article by Adam Grant in the New York Times (19th April 2021) hit the nail on the head. He describes a feeling of ‘languishing’. Not depressed, but not thriving; a sense of stagnation and emptiness, of muddling through days feeling joyless and aimless. He described languishing as the neglected middle child of mental health, the void between depression and flourishing – the absence of well-being. How many people are languishing and how long will it be before they are thriving? One suspects that a languishing epidemic is upon us, with no imminent cure in sight.
What’s ahead and what role for pharma?
In healthcare, as in strategic planning, we are at risk of overestimating the impact of short-term threats and underestimating the impact of long-term threats. We see what is immediately in front of us, but we are not good at imagining what might be. We have all been so busy following new Covid-19 diagnoses, deaths and variants of concern that we have not yet stopped to really consider where we should go from here. We see the wave, but not the ripple and certainly not the tsunami.
To my mind, the pharmaceutical industry has a major role to play in supporting recovery in all of these areas. Really? How?
In the absence of the NHS workforce expanding exponentially, clearing the backlog of patients waiting to be treated across a host of clinical conditions will need service provision to be reimagined. The Planning Guidance for 2021/22 sets out how the NHS will restore services. Along with delivering the strategic goals of the Long Term Plan, the following priorities have been identified:
- Staff health and wellbeing, recruitment and retention
- Covid vaccination and meeting needs of patients with Covid-19
- Transform service delivery, accelerate elective and cancer service restoration, and manage increasing demand on mental health services.
- Expand primary care capacity to improve access, outcomes and address health inequalities
- Transform community, urgent and emergency care, timely admission and reduced length of stay
- Collaborative working
“From a healthcare perspective the ripples of Covid-19 will be felt for years, perhaps even decades.”
The planning guidance sets out the way forward for hospitals:
- Recover activity towards previous levels
- Produce delivery plans for elective inpatient, outpatient and diagnostic services (including specialised services)
- Maximise available physical and workforce capacity across each system
- Consider high-impact changes – adapting ward environments to enhance flow, patient segregation and service transformation initiatives
- Prioritise the clinically most urgent patients
- Clinically-led review and validation of waiting lists
- Effective communication with patients – proactive approach to vulnerable patients
- Address the longest waiters and tackle health inequalities
“In healthcare, as in strategic planning, we are at risk of overestimating the impact of short-term threats and underestimating the impact of long-term threats.”
A fresh take on goals and treatment outcomes?
More than ever, services will need to consider adopting treatment approaches that improve service efficiency, increase capacity and reduce length of stay. We need to consider refocusing our messages, so long obsessed with budget impact, to incorporate these.
That’s not to say that cost will not continue to be important, because of course it will. Although £6.6 billion in additional funding, including a £1 billion Elective Recovery Fund, sounds like a lot, it won’t go as far as we think. Budgets will continue to be stretched and we will need to consider this in our marketing strategies.
“More than ever, services will need to consider adopting treatment approaches that improve service efficiency, increase capacity and reduce length of stay.”
We need to have an eye on the evolving financial flows and payment systems in the NHS in England. The dust has yet to settle, but it’s very much looking like Payment by Results has had its day. Some might say about time too. We all know that it never was about results but about activity. To play devil’s advocate, payment based on activity might be exactly what we do need, but that ship may have sailed!
Services are being encouraged to learn from other systems. Traditionally the NHS is reluctant to adopt solutions developed elsewhere in the system. There is a tendency to adopt a ‘not invented here’ mentality and to justify it based on service differences, rather than looking to see the similarities.
Surely pharma marketing is uniquely placed to support this process, with the in-depth knowledge that our field-based teams have on services? Perhaps at this juncture, if we approach it in the right way, we will find a receptive audience desperate for any help they can get in dealing with the post Covid-19 tsunami.