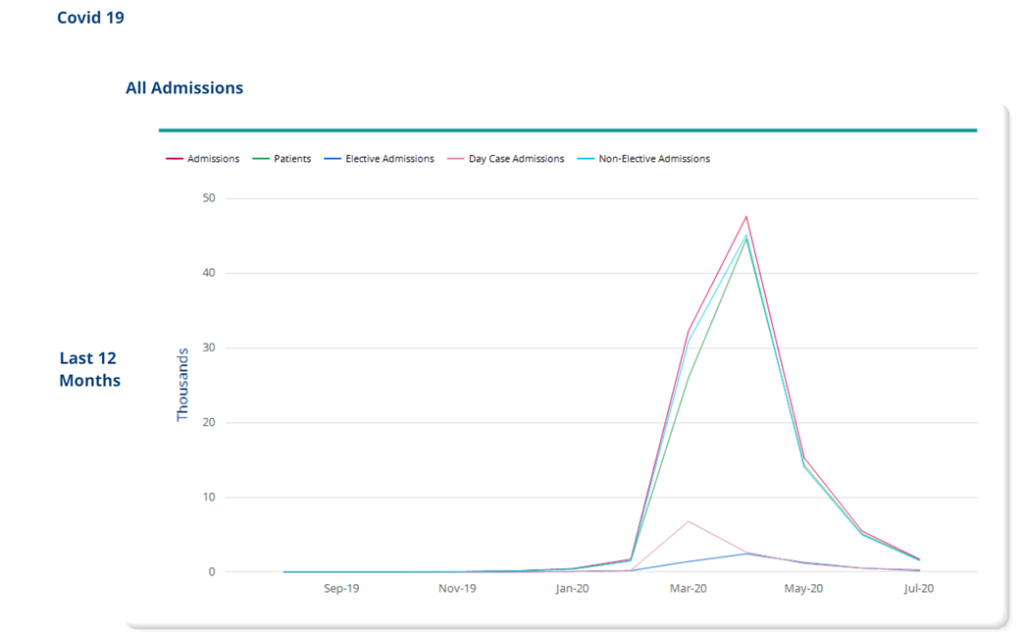
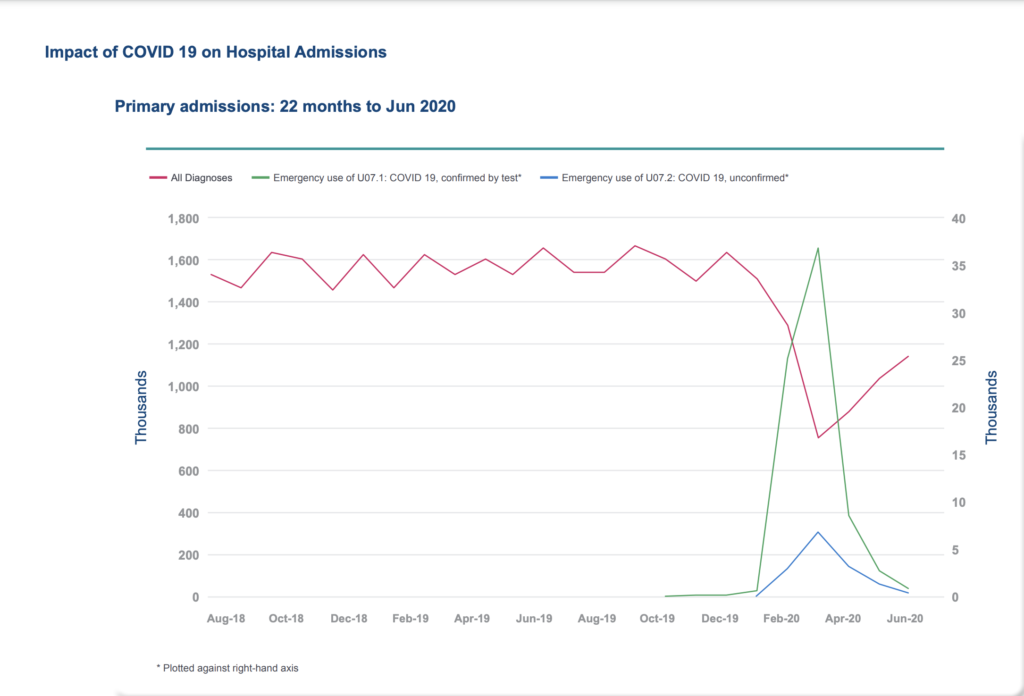
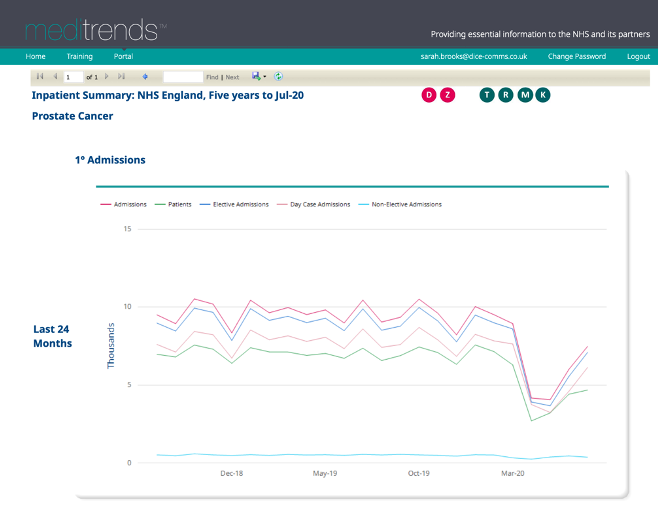
The COVID-19 Pandemic has had a huge impact on the treatment of long-term and chronic conditions, and we have seen a reduction in hospital activity for non-COVID related conditions.
From HES data we have measured the impact on these services.
We can see from the HES data that nationally in January 2020 there were 5,510 admissions with a primary diagnosis of MS and that that figure dropped to just 3,140 admissions in April 2020. A reduction of 36% at the height of the COVID-19 pandemic, during the period of full national lockdown.
The number of admissions for this cohort of patients increased slightly in May 2020 to 3,390 and by July the number had increased to 4,895. A significant increase from April but numbers had still not returned to the same level as pre-lockdown.
The decrease of patients with a diagnosis of MS in any diagnosis position is even more significant. In January 2020 there were 10,435 admissions of patients with a diagnosis of MS in any position and this decreased by 48% by April, when there were just 5,415 admissions for this cohort of patients.
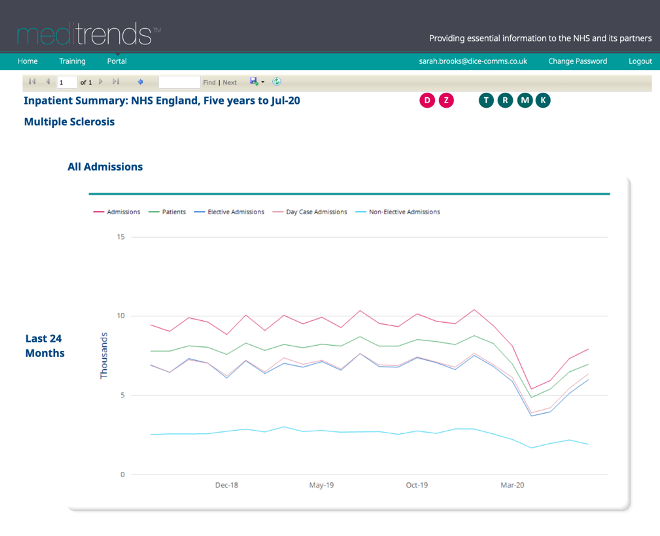
The number of admissions relating to this cohort of patients increased to 7,940 in July 2020, but this is still 24% less than the number of admissions in January – before the COVID-19 pandemic began.
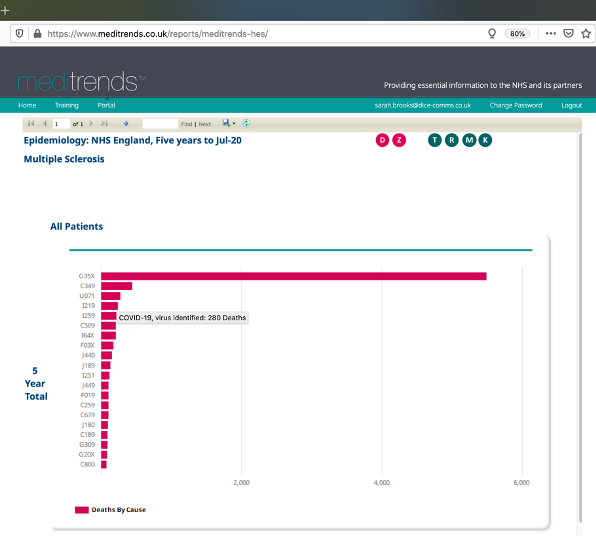
Mortality:
COVID-19 is stated as the second highest cause of death in patients admitted with a primary diagnosis of MS in the last 5 years, with a total of 65 deaths attributed to the U071 ICD10 code- the emergency code used for COVID-19.

For patients admitted with a diagnosis of MS in ‘any’ diagnosis position COVID-19 was the third highest cause of death, with 280 deaths recorded against ICD10 code U071 (COVID 19)
Please note, due to the way MS is coded in HES, we are unable to differentiate between relapsing-remitting MS (RRMS), primary progressive MS (PPMS) and secondary progressive MS (SPMS).
To find out more about the impact COVID-19 has had on patients with a diagnosis of MS – or to obtain similar insights relating to your disease or therapy area, please contact Sarah Brooks (Sarah.brooks@dice-comms.co.uk)